Our Focus
Targets
© UNFPA Chad/Liga Nassandou. UNFPA humanitarian midwives, Sylvie Hadjé (left) and Mariam Tcheré (right), pictured with Maimouna Mahamat and her newborn baby, at a health centre in Djabal refugee camp in Eastern Chad.
Home > Accelerate maternal and newborn survival and wellbeing > The Targets
We know what works to greatly improve the survival of pregnant women, mothers, newborns and babies.
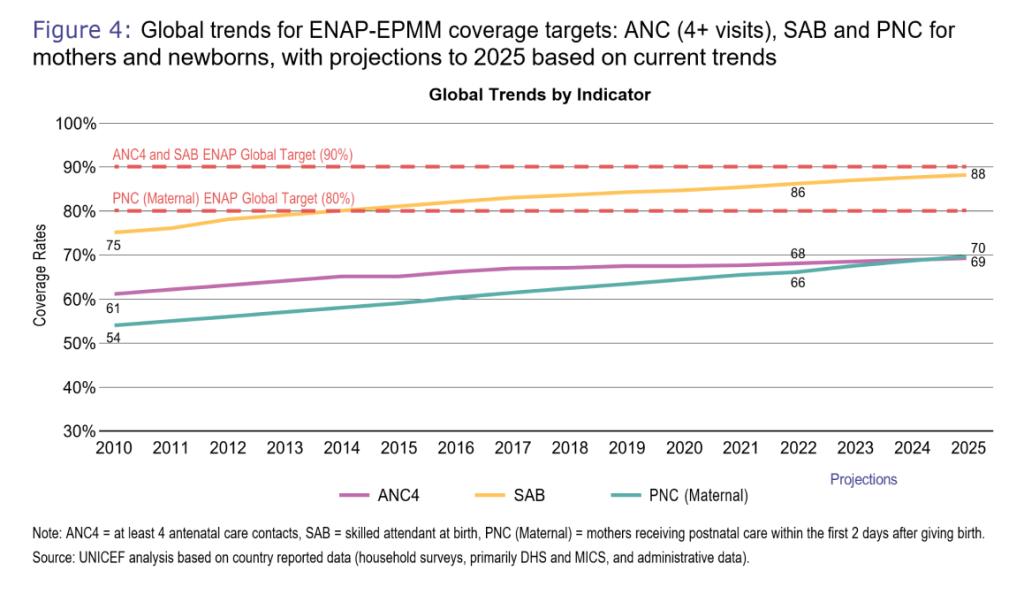
Every Woman Every Newborn Everywhere (previously ENAP EPMM) has set ambitious population coverage targets for critical high impact intervention packages of care to drastically reduce the mortality of pregnant women, new mothers and newborns, and prevent stillbirths. They require high coverage of lifesaving interventions during pregnancy, birth and the early weeks after birth, combined with quality and equity, and a focus on the care of small and sick newborns and women with obstetric complications. [1]
Link: The antenata period presents opportunities,interventions
©UNFPA
Target 1
Status
Target 2
Status
Target 3
Status
Target 4
Status
Growing proportion of women who make their own informed and empowered decisions about their sexual and reproductive health.
Impact
Every Woman Every Newborn Everywhere set global but also national and subnational targets. These are particularly important because national averages can mask wide intra-country disparity. Progress is assessed not only in terms of national averages, but also on how gains benefits all groups living in a country. Disaggregating data to subnational levels can reveal specific areas with low coverage, helps identifying vulnerable populations, and facilitates evidenced-based policy making to improve the health of women, mothers and babies.
Why these targets?
Because we know what interventions do improve maternal and newborn survival and health, and reduce stillbirths.
©WHO/Neil Nuia
Lottie and her child at the postnatal ward at National Referral Hospital in Honiara, Solomon Islands in 2022.
Antenatal care visits:
Why it matters: Antenatal care models with a minimum of eight contacts are recommended to reduce perinatal mortality and improve women’s experience of care. As there was no data collected on eight visits, the coverage target is set at four antenatal care visits.Receiving antenatal care at least four times increases the likelihood of reaching pregnant women with interventions that may be vital to their health and wellbeing and that of their infants, and reduce the risks of stillbirths and pregnancy complications.
Resource: WHO recommendations: intrapartum care for a positive childbirth experience
Women and their babies are attended in the 2 days following birth
Why it matters: Up to 30% of maternal deaths occur postpartum. During postnatal care visits, health workers can identify risks, prevent complications for both the mother and the newborn, promote their health and wellbeing, foster support from the family and the community and address health-related and social needs.
Resource: WHO recommendations on maternal and newborn care for a positive postnatal experience
©WHO/Yoshi Shimizu
A health worker gives a vaccination to a baby at a family health center in Kiribati in 2019.
Small and sick newborns have access to specialized care
Why it matters: Small and sick newborns are at the greatest risk of death and disability. A total of 30 million newborns per year require some level of specialized or intensive care in hospitals around the world[2]
Link: Births attended by skilled health personnel
. Of those that do survive, many do with lifelong conditions and disabilities that are preventable. If all countries achieved care for small and sick newborns with quality, over 740 000 lives could be saved every year.[3]
Link: https://newborntoolkit.org/problem
Resource: Survive and thrive: transforming care for every small and sick newborn
©WHO/Fanjan Combrink
A nurse vaccinates Gertrude’s son at the Child Welfare Clinic at St Francis Xavier Hospital in Assin Fosu, Central Region, Ghana in 2023.
Emergency obstetric care services are available and functioning
Why it matters: While most pregnancies and births are uneventful, all pregnancies are at risk. Around 15% of all pregnant women will develop a potentially life-threatening complication that calls for skilled care, and some will require a major obstetrical intervention to survive[4]
Link: https://www.who.int/publications/i/item/WHO-MCA-17.02
. In addition, an estimated 45% of all stillbirths occurred during labour in 2021[5]
Link: https://data.unicef.org/topic/child-survival/stillbirths/
. Access to high-quality care during childbirth, including ongoing intrapartum monitoring and timely intervention in case of complications, is essential.
©UNICEF/U.S. CDC/Saiyna Bashir
Staff nurse Mariam Azam holds 6-hour-old Muhammad Awais in a dedicated room for vaccination, in April 2023 at the Ganga Ram Hospital in Lahore, Punjab province, Pakistan.
Women decide on their sexual and reproductive health
©WHO/Hickmatu Leigh. Magdalene (left) tutors a newly admitted midwifery student, Massah (right), about family planning methods, specifically the use of male and female condoms.
Trends
Current trends below show that we will fall short of these targets by 2025: